Machine learning (ML) has the potential to revolutionize the way respiratory diseases are detected and diagnosed. By combining cough sound analysis with computed tomography (CT) and chest radiography (CXR), ML algorithms can efficiently detect a wide range of conditions, including COVID-1924,25.
Such methods have already been used in the past to diagnose and predict the outcome of conditions such as lung cancer, bronchitis, pneumonia, COPD, TB and asthma5,17,26,27,28,29,30,31.
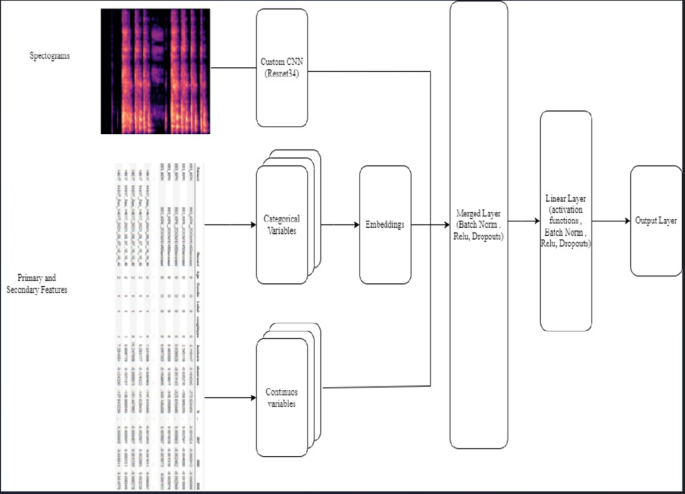
AI has the potential to improve respiratory health by providing faster and more accurate diagnoses. AI algorithms can analyse large data sets to identify patterns and trends that help in developing new treatment methods. Our contribution to the State of the art is the Swaasa AI platform that combines the final output layers of two separate models – a tabular model that uses the primary and secondary features as input and a CNN model that used MFCC spectrograms as input. This approach resulted in significantly better predictions than previously used logistic regression or a CNN model alone17,30,31.
In our cross-sectional feasibility study, we evaluated the usability and efficacy of “Swaasa” for rapid respiratory health assessment. The study specifically focused on analysing cough patterns and using risk classifiers to assess respiratory health. The risk classifier, trained using cough data, accurately determines the risk of respiratory disorders, classifying it as “Yes” or “No.” This allows for early identification of individuals who may require further evaluation and medical intervention. The pattern classifier, also trained on cough data, categorizes coughs into three types: obstructive, restrictive, and mixed, providing valuable insights into the underlying respiratory conditions. Together, these classifiers enable a comprehensive assessment of respiratory health, facilitating timely interventions and personalized treatment plans. Also, the clinical validation was conducted on a relatively large cohort, whereas previous studies were carried out on smaller scales or using unreliable crowdsource datasets17,30,32. This approach provided a more robust and reliable dataset for evaluation.
Model’s risk classifier plays a crucial role in identifying individuals at risk of respiratory disorders. By analysing cough patterns, the platform accurately determines the likelihood of respiratory issues, such as obstructive, restrictive, and mixed conditions. The study revealed that the risk classifier of the Swaasa platform achieved a sensitivity of 97.27%, indicating its high capability in correctly identifying individuals who are at risk. This sensitivity implies that the risk classifier has a low rate of false negatives, effectively detecting a significant proportion of individuals with potential respiratory disorders. The accurate identification of at-risk individuals enables timely interventions and targeted healthcare strategies to improve their overall respiratory health outcomes. The results of the assessments obtained using the model were found to be highly correlated with those obtained from traditional methods, indicating that the platform can accurately assess respiratory health. The results of the study also showed that the predictions made by pulmonologists regarding respiratory disease patterns matched well with the outcomes generated by the Swaasa system. This was demonstrated by a moderate level of agreement, as measured by the interrater variability value (κ = 0.607). This indicates that the predictions made by pulmonologists and the outcomes generated by Swaasa system were consistent, which is important validation of the accuracy and reliability of the system.
The present study establishes the feasibility and safety of implementing the Swaasa AI platform for respiratory health assessment in primary healthcare settings. Through a comprehensive evaluation involving Critical Task Analysis and a Questionnaire survey, valuable insights were gained regarding the platform’s usability and efficacy. The study identified important safety considerations, including the need for standardized cough recording protocols, mitigation of potential adverse effects, management of background noise during audio recording, and implementation of appropriate device cleaning procedures. Usability enhancements were recommended, particularly in addressing screen navigation and session expiry issues. Additionally, the study highlighted the high level of user satisfaction, with participants expressing positive feedback regarding the platform’s simplicity, ease of use, and consistency. These findings reinforce the potential of the Swaasa AI platform as a valuable tool for respiratory health assessment in primary healthcare, while also providing valuable guidance for further refinement and optimization.
In conclusion, the model demonstrates the feasibility and efficacy of utilizing cough patterns and risk classifiers for rapid respiratory health assessment. Its potential applications extend to primary care clinics, hospitals, and remote locations, where it can significantly enhance the speed and accuracy of respiratory health evaluations. Furthermore, the platform serves as a valuable triage tool, enabling the identification of high-risk patients and optimizing the allocation of clinical resources for improved patient outcomes.
To ensure the generalizability of the Swaasa platform, future studies will involve mass screening of subjects from diverse populations, languages, and cultures. This approach will validate its effectiveness and applicability across various settings globally. Additionally, efforts will be made to diversify the training data set, incorporating a wider range of respiratory conditions and demographics, further enhancing the platform’s accuracy and reliability.
Safety and usability considerations are integral to the continuous development and implementation of the model. Strict adherence to safety guidelines, including the standardization of cough recording protocols, mitigation of potential adverse effects, management of background noise, and appropriate device cleaning procedures, ensures the safety of both patients and healthcare providers. Ongoing refinements will address usability aspects such as screen navigation and session expiry issues, aiming to optimize user experience and facilitate seamless integration of the platform into routine clinical practice.
Overall, the model demonstrates promise as an efficient and reliable screening tool for respiratory health assessment, with future advancements and validations anticipated to further establish its utility in diverse healthcare settings.
link