Respiratory diseases statistics – Statistics Explained

Data extracted in October 2023.
Planned article update: 22 November 2024.
Highlights
Diseases of the respiratory system accounted for 6.7 % of all deaths in the EU in 2020.
In 2021, at least three quarters of all people aged 65 years and over in Ireland and Denmark had been vaccinated against influenza, the highest shares among the EU Member States.
On average in 2021, in-patients with diseases of the respiratory system spent between 5.2 days (the Netherlands) and 12.0 days (Czechia) in hospital.
This article presents an overview of European Union (EU) statistics related to diseases of the respiratory system and focuses on deaths from diseases of the respiratory system and healthcare for diseases of the respiratory system.
The respiratory system is a series of organs that are responsible for breathing; the lungs are the primary organ of this system, which also includes the nasal passage, oral cavity, pharynx, larynx, trachea, bronchi and bronchioles. Diseases of the respiratory system are one of the main causes of death in the EU and include conditions such as chronic obstructive pulmonary disease, pneumonia or asthma. Note that the statistics presented in this article do not cover cancer of the respiratory system (such as lung cancer), which is treated in a separate article.
This article is one of a set of statistical articles concerning health status in the EU which forms part of an online publication on Health in the European Union – facts and figures.
Most of the data in this article relate to 2020 or 2021, although there are some data for earlier reference periods: as such, this article includes data that may have been impacted by the COVID-19 pandemic and its related restrictions. For this reason, particular attention should be paid when comparing the 2020 and/or 2021 data with data from earlier years. COVID-19 is a respiratory disease caused by the SARS-CoV-2 coronavirus. Note that COVID-19 was included as a main cause of death from 2020 onwards and that this may have resulted in a lower number of deaths caused by (other) respiratory diseases.
In some EU Member States, healthcare resources were placed under intense pressure (particularly at the start of the pandemic) from an influx of patients with COVID-19. The pandemic also resulted in a range of knock-on effects including, among others, some services being curtailed/postponed due to the number of COVID-19 patients, staff shortages within hospitals and day care centres due to infection/quarantine procedures, and patients being hindered accessing medical services due to their own infection/quarantine as well as lockdown or travel restrictions.
Deaths from diseases of the respiratory system
Diseases of the respiratory system accounted for 6.7 % of all deaths in the EU in 2020
In 2020, there were 347 867 deaths in the EU resulting from diseases of the respiratory system, equivalent to 6.7 % of all deaths among residents. Table 1 shows that, in 2020, the proportion of deaths in Malta, Denmark and Ireland from respiratory diseases was considerably higher than the EU average, at 10.5 %, 10.4 % and 10.0 %, respectively. At the other end of the range, respiratory diseases were the main cause of death for less than 3.5 % of the population in Slovenia, Finland and the Baltic Member States.
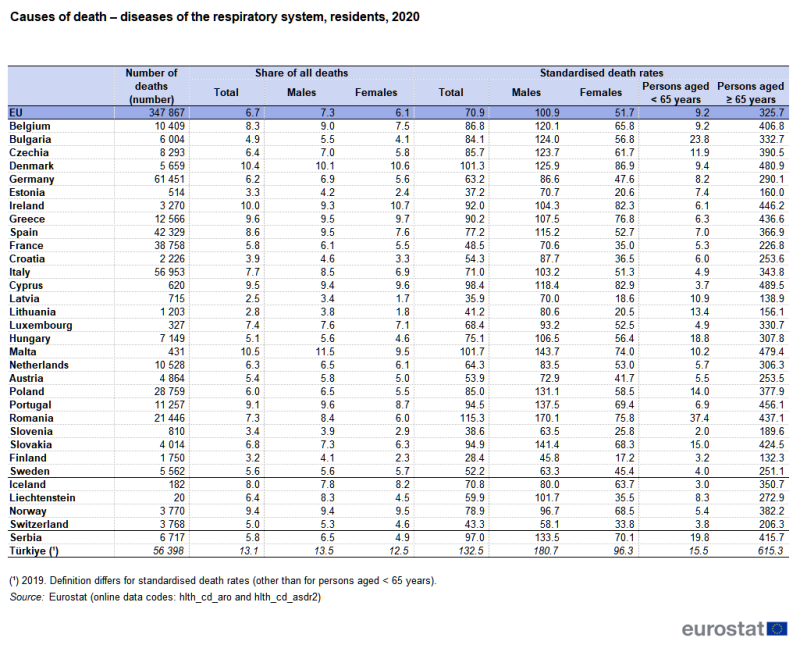
Across the EU, a higher proportion of males than females died from diseases of the respiratory system (7.3 % compared with 6.1 %) in 2020. This situation was repeated in most of the EU Member States. The difference was most pronounced in Romania (where the gender gap was 2.4 percentage points (pp)), while Lithuania and Malta had shares for males that were 2.0 pp higher than those for females. By contrast, a higher proportion of deaths among females (rather than males) were attributed to diseases of the respiratory system in five Member States, with the largest gender gap in Ireland (1.4 pp).
Standardised death rates for respiratory diseases were higher for males than for females
The EU’s standardised death rate for diseases of the respiratory system was 70.9 deaths per 100 000 inhabitants in 2020; the death rate for males (100.9 deaths per 100 000 male inhabitants) was almost twice as high as that for females (51.7 deaths per 100 000 female inhabitants). Standardised death rates for males were higher than those for females in 2020 in each of the EU Member States. The gender difference may, at least in part, be attributed to different smoking habits between the sexes or to occupational risks (for example, more males work(ed) in extractive industries such as coal mining). Death rates for males were at least three times as high as those for females in all three Baltic Member States, while elsewhere they were between 1.3 and 2.7 times as high. The smallest gender gaps (in relative terms) were recorded in Ireland, Sweden, Greece, Cyprus and Denmark, with standardised death rates for males for respiratory diseases that were 1.3 or 1.4 times as high as those for females.
Table 1 shows that standardised death rates for diseases of the respiratory system were particularly concentrated among older people. This underlines the concern over winter influenza epidemics within elderly populations. The EU’s standardised death rate for respiratory diseases among people aged 65 years and over was 35 times as high as the standardised death rate for people aged less than 65 years. This was considerably higher than the same ratio for all causes of death, where the standardised death rate for the older age group was 22 times as high (as that for the younger age group).
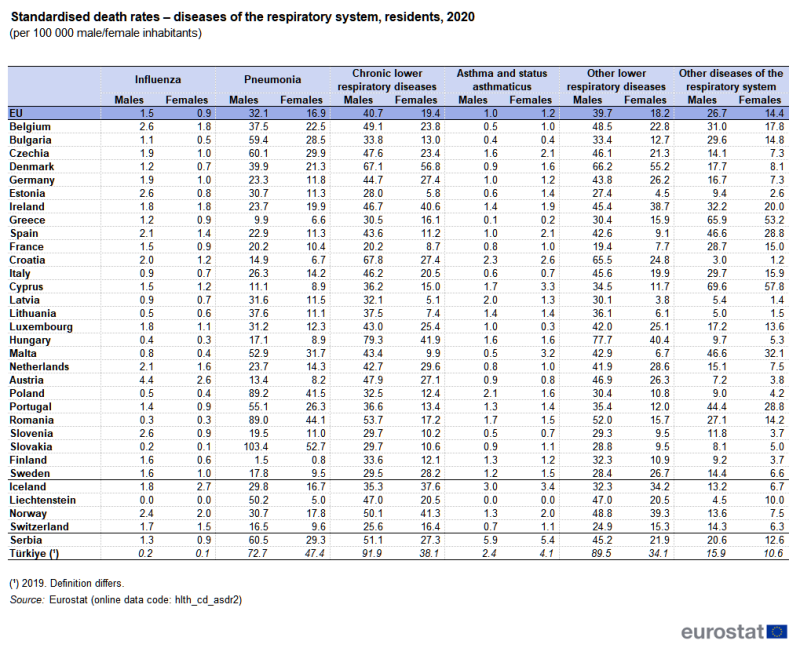
A more detailed analysis of causes of death for diseases of the respiratory system is presented in Table 2. It shows the main causes of death among respiratory diseases were lower respiratory diseases (chronic or other) and pneumonia, while standardised death rates for asthma and for influenza were considerably lower.
(per 100 000 male/female inhabitants)
Source: Eurostat (hlth_cd_asdr2)
In 2020, the highest standardised death rates for chronic lower respiratory diseases among the EU Member States were recorded in Denmark and Hungary, while the highest rates for pneumonia were registered in Slovakia, Romania and Poland. Among the diseases with much lower mortality rates, Cyprus and Croatia recorded the highest standardised death rates for asthma and status asthmaticus (also known as acute severe asthma), while Austria had the highest standardised death rate for influenza.
The standardised death rate for asthma was higher among females
With the exception of asthma and status asthmaticus, EU standardised death rates for males in 2020 were higher than those for females for each of the causes of death presented in Table 2. Gender differences were most pronounced for other lower respiratory diseases and chronic lower respiratory diseases as the standardised death rates for males in the EU were 2.2 and 2.1 times as high as the corresponding rates for females. There was only one exception where rates were higher for females than for males: for influenza in Lithuania.
In 2020, the EU standardised death rate for asthma and status asthmaticus was higher for females (1.2 deaths per 100 000 female inhabitants) than the corresponding rate for males (1.0 deaths per 100 000 male inhabitants). This difference between the sexes was largest in Malta, where the female standardised death rate for asthma and status asthmaticus was 6.4 times as high as that recorded for males. Large relative differences were also observed in Greece, Estonia and Spain, where the female death rate was more than twice as high as the male rate. There were nine EU Member States where the death rate for asthma and status asthmaticus was higher for males than for females: among these, the rates were relatively similar for both sexes, except in Latvia and Luxembourg.
Self-reporting of respiratory diseases
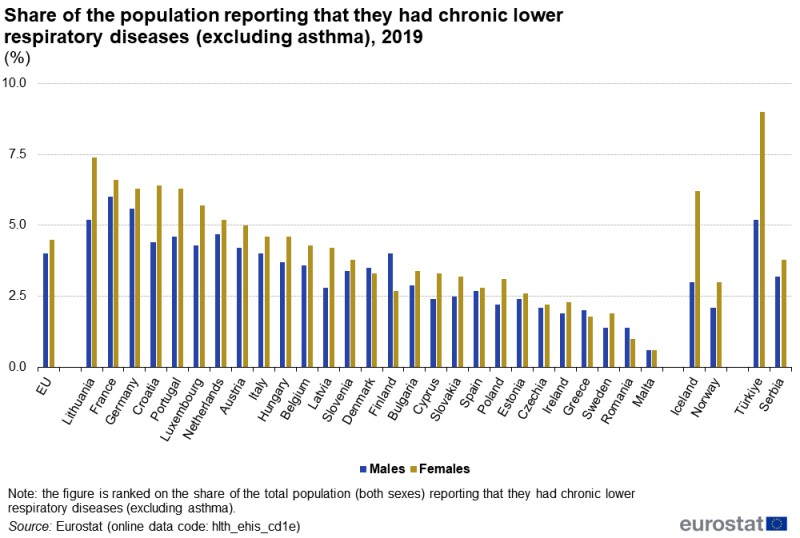
The data presented in Figures 1 and 2 are derived from the third wave of the European health interview survey (EHIS) which covered persons aged 15 years and over. The survey included questions asking respondents to self-assess their own health, including whether they had a chronic lower respiratory disease (excluding asthma).
People in Lithuania reported the highest prevalence of chronic lower respiratory diseases (other than asthma)
Chronic lower respiratory diseases (excluding asthma) cover a collection of lung diseases that include chronic bronchitis, emphysema and other chronic obstructive pulmonary diseases; the main cause of these diseases being smoking. Patients with chronic lower respiratory diseases have difficulties in breathing, as the walls of the airways to their lungs are damaged, scarred and narrowed (airflow obstruction).
In 2019, some 4.3 % of the EU population aged 15 years and over stated that they had some form of chronic lower respiratory disease (other than asthma) diagnosed by a medical doctor (see Figure 1). Lithuania (6.4 %) recorded the highest share among the EU Member States, followed by France, Germany, Croatia, Portugal, Luxembourg and the Netherlands – each with shares of at least 5.0 %. At 7.1 %, the share in Türkiye was considerably higher than in any of the EU Member States. By contrast, less than 2.0 % of the population in Greece, Sweden, Romania and Malta declared that they suffered from chronic lower respiratory diseases (other than asthma).
(%)
Source: Eurostat (hlth_ehis_cd1e)
An analysis by sex reveals that females aged 15 years and over were usually more likely to report that they had chronic lower respiratory diseases than males. In 2019, 4.5 % of females in the EU reported such an illness, compared with 4.0 % of males. This gender difference was particularly pronounced in Lithuania, Croatia and Portugal, where the gap between the sexes was 2.2, 2.0 and 1.7 pp, respectively. By contrast, the proportion of males reporting such an illness was greater than that for females in Finland (1.3 pp higher), Romania, Denmark and Greece; in Malta, the shares were the same for males and females.
Across the EU Member States, the highest share of the female population reporting in 2019 that they suffered from a chronic lower respiratory disease (other than asthma) was observed in Lithuania (7.4 %). The highest proportion among males was recorded in France (6.0 %).
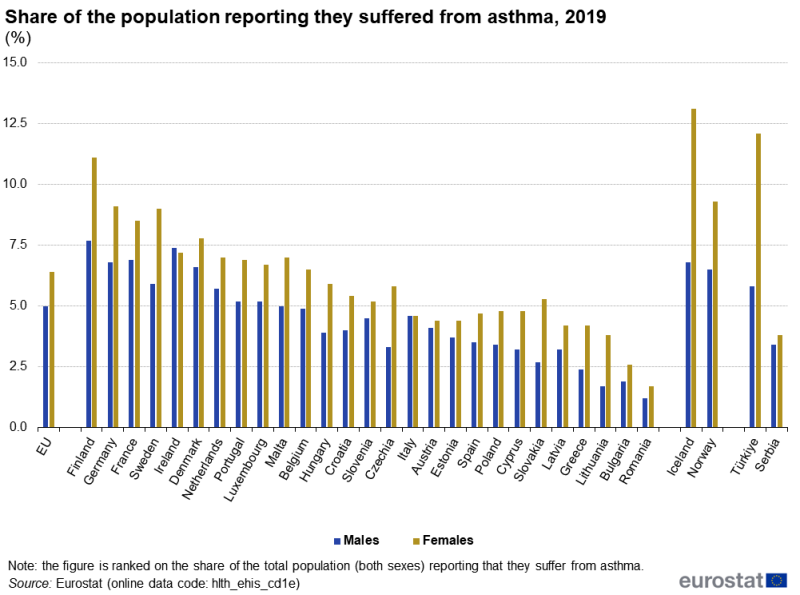
The prevalence of asthma was highest in Finland
Asthma is a chronic inflammation of the airways characterised by reversible airflow obstruction and bronchospasm that can cause coughing, wheezing, chest tightness or a shortness of breath. It may result from a range of triggers, which include (among others): pollution, tobacco smoke, solvents, pollens, cold air or strenuous exercise.
In 2019, some 5.7 % of the population aged 15 years and over in the EU reported that they suffered from asthma. The highest share of self-reported asthma across the EU Member States was recorded in Finland (9.4 %), where 11.1 % of females and 7.7 % of males stated that they had asthma (see Figure 2). The next highest overall shares (for both sexes) were in Germany (8.0 %), France (7.8 %) and Sweden (7.5 %). The share of females in the EU reporting that they suffered from asthma was 6.4 %, which was 1.4 pp higher than the corresponding share recorded among males (5.0 %).
A closer analysis of the 2019 data reveals that a higher proportion of females (than males) declared they had asthma in all of the EU Member States except for Ireland and Italy; the share (7.4 %) of males in Ireland who declared they had asthma was 0.2 pp higher than the share for females; in Italy, the shares for both sexes were the same (4.6 %). By contrast, in Finland, Sweden, Slovakia, Czechia, Germany, Lithuania, Hungary and Malta the shares for females were at least 2.0 pp higher than those for males, peaking at a difference of 3.4 pp in Finland.
(%)
Source: Eurostat (hlth_ehis_cd1e)
Preventive care – vaccination
Three quarters of persons aged 65 years and over in Ireland and Denmark were vaccinated against influenza
It may be argued that many of the deaths and some of the costs associated with influenza epidemics could be avoided through a wider uptake of influenza vaccinations. Among the EU Member States, there is a range of different policies with respect to making influenza vaccines available to the general public. Often these vaccines are targeted at older age groups or other at-risk groups.
Figure 3 shows the take-up of vaccinations against influenza among people aged 65 years and over: there are considerable differences between EU Member States. At least three quarters of people aged 65 years and over in Ireland and Denmark were vaccinated against influenza in 2021, as were 72.6 % in the Netherlands. By contrast, no more than 10.0 % of the elderly population were vaccinated against influenza in Latvia, Bulgaria and Poland.
In 21 of the EU Member States for which data are presented (see Figure 3 for more information on the coverage), the share of the elderly vaccinated against influenza was higher in 2021 than it had been in 2011. The proportion of the population aged 65 years and over that was vaccinated against influenza was more than 20 pp higher in 2021 than in 2011 in Denmark, Finland and Estonia. By contrast, the share of the population aged 65 years and over that was vaccinated fell 9.0 pp in Slovakia and 11.3 pp in Germany (2013–2021; note there is a break in series with coverage being extended to people aged 60 years and over for the latest reference period).
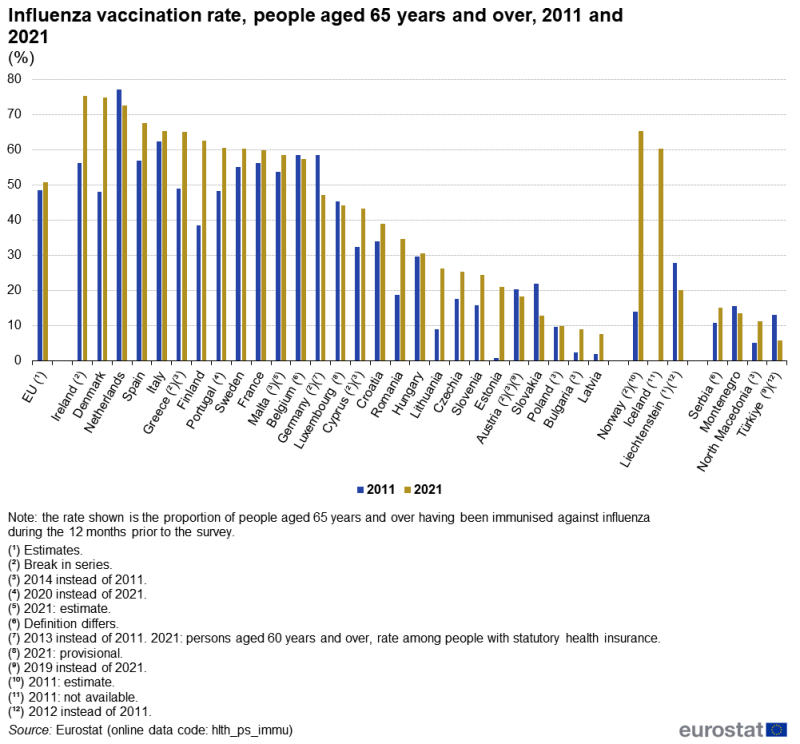
(%)
Source: Eurostat (hlth_ps_immu)
In-patient respiratory healthcare
In 2021, approximately 4.2 million in-patients with diseases of the respiratory system were discharged from EU hospitals
Across the EU in 2021 (2020 data for Belgium and Malta; no recent data for Denmark, Greece and Luxembourg), in-patients with diseases of the respiratory system (codes J00–J99) spent a total of 34.5 million days in hospital. By far the highest number of in-patient days was spent in German hospitals (26.6 % of the EU total), while Italy (12.6 %) was the only other EU Member State to record a double-digit share.
Around 4.2 million in-patients with diseases of the respiratory system were discharged from EU hospitals in 2021 (2020 data for Belgium and Malta; no recent data for Denmark, Greece and Luxembourg). Discharges of in-patients treated for respiratory diseases accounted for 17.5 % of the total number of hospital in-patient discharges in Cyprus and 16.6 % in Romania, while these diseases also accounted for double-digit shares of all in-patient discharges in Slovenia, Lithuania, Ireland, Belgium (2020 data), Estonia, Slovakia and Czechia. By contrast, respiratory diseases accounted for a relatively low proportion of the total number of in-patient discharges in France (3.4 %).
Additional information on this topic is available in the article Hospital discharges and length of stay statistics.
Lithuania, Romania and Bulgaria had highest number of in-patient discharges per 100 000 inhabitants
Relative to population size, Lithuania, Romania and Bulgaria recorded the highest in-patient discharge rates among those treated for diseases of the respiratory system in 2021 (see Figure 4), each in excess of 1 800 per 100 000 inhabitants. Hungary and the Netherlands had the lowest in-patient discharge rates for diseases of the respiratory system, both fewer than 600 per 100 000 inhabitants.
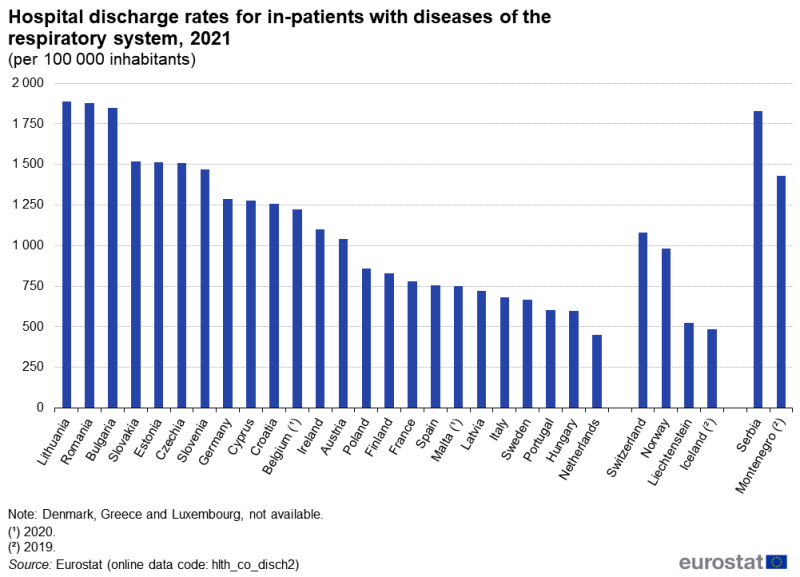
(per 100 000 inhabitants)
Source: Eurostat (hlth_co_disch2)
The length of hospital stays for in-patients with diseases of the respiratory system was generally close to the average for all types of disease
Table 3 presents an analysis of the average length of hospital stays for in-patients treated for a respiratory disease in 2016 and 2021. The average hospital stay in 2021 ranged in length from 5.3 days in Sweden and 5.2 days in the Netherlands up to 10.8 days in Italy and a peak of 12.0 days in Czechia. In France, the average length of a hospital stay for those treated for a disease of the respiratory system was 2.5 days shorter than the average for all diseases. Aside from France, the average length of a hospital stay due to a disease of the respiratory system was similar to the average for all diseases in most of the EU Member States, as this difference ranged between 1.6 days shorter for diseases of the respiratory system (Hungary) to 1.3 days longer (Romania). However, there were six Member States that reported that the average length of a hospital stay due to a disease of the respiratory system was at least 2.0 days longer than the average for all diseases. The largest differences were observed in Belgium (2.6 days; 2020 data), Slovenia (also 2.6 days) and Czechia (2.5 days).
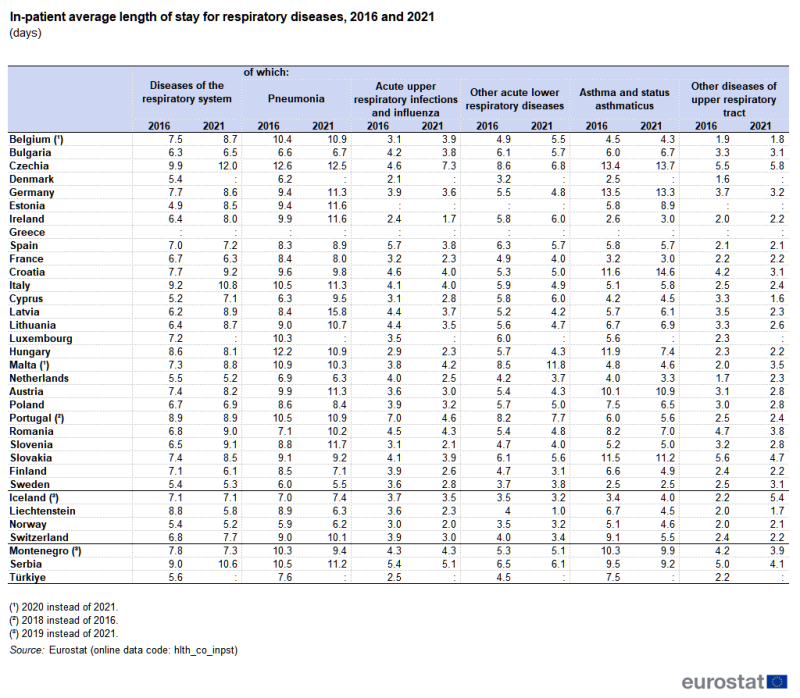
(days)
Source: Eurostat (hlth_co_inpst)
Among the 24 EU Member States for which comparable data are available (incomplete or no data for Denmark, Greece and Luxembourg), the average length of a hospital stay for in-patients treated for a disease of the respiratory system increased between 2016 and 2021 in 18, was unchanged in Portugal (2018–2021), and fell in the remaining five. The largest decrease between 2016 and 2021 in the average time spent in hospital for in-patients treated for a disease of the respiratory system was 1.0 day in Finland. By contrast, Estonia, Latvia and Slovenia recorded the largest increases, up 3.6 days, 2.7 days and 2.6 days, respectively.
The remainder of Table 3 provides a more detailed analysis of the average length of hospital stays for in-patients diagnosed with five different types of respiratory diseases. On average, in-patients with pneumonia (codes J12–J18) and with asthma and status asthmaticus (codes J45–J46) spent the largest number of days in hospital. These figures are of interest, insofar as pneumonia was one of the leading causes of death among respiratory diseases, in contrast to asthma, which has a death rate that was relatively low. The average stay in hospital for in-patients being treated for asthma varied considerably across the EU Member States, from a high of 14.6 days in Croatia to no more than 3.0 days in Sweden, Ireland and France.
Source data for tables and graphs
Key concepts=
An in-patient is a patient who is formally admitted (or ‘hospitalised’) to an institution for treatment and/or care and stays for a minimum of one night or more than 24 hours in the hospital or other institution providing in-patient care. An in-patient or day care patient is discharged from hospital when formally released after a procedure or course of treatment (episode of care). A discharge may occur because of the finalisation of treatment, signing out against medical advice, transfer to another healthcare institution, or because of death.
The number of deaths from a particular cause of death can be expressed relative to the size of the population. A standardised (rather than crude) death rate can be compiled which is independent of the age and sex structure of a population: this is done as most causes of death vary significantly by age and according to sex and the standardisation facilitates comparisons of rates over time and between countries.
Healthcare resources and activities
Statistics on healthcare activities (such as information on hospital discharges) are documented in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
For hospital discharges and the length of stay in hospitals, the international shortlist for hospital morbidity tabulation (ISHMT) is used to classify data from 2000 onwards; Chapter X covers diseases of the respiratory system.
- Acute upper respiratory infections and influenza (1001)
- Pneumonia (1002)
- Other acute lower respiratory infections (1003)
- Chronic diseases of the tonsils and adenoids (1004)
- Other diseases of upper respiratory tract (1005)
- Chronic obstructive pulmonary disease and bronchiectasis (1006)
- Asthma (1007)
- Other diseases of the respiratory system (1008)
For country specific notes on these data collections, please refer to the annexes at the end of the national metadata reports accessible from links at the beginning of the European metadata report.
The Healthcare non-expenditure statistics manual provides an overview of the classifications, both for mandatory variables and variables provided on voluntary basis.
Health status
Self-reported statistics covering the health status of the population for a range of chronic diseases are provided by the European health interview survey (EHIS). This source is documented in more detail in the background article European health interview survey – methodology which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions. The data presented in this article refer to the share of the population aged 15 years and over reporting to have been diagnosed by a medical doctor with chronic bronchitis, chronic obstructive pulmonary disease, emphysema, or asthma (allergic asthma included) during the 12 months prior to the survey.
Causes of death
Statistics on causes of death provide information on mortality patterns, supplying information on developments over time in the underlying causes of death. This source is documented in more detail in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Causes of death are classified according to the European shortlist (86 causes), which is based on the International Statistical Classification of Diseases and Related Health Problems (ICD). Chapter X of the ICD covers diseases of the respiratory system.
- J00–J06 Acute upper respiratory infections
- J09–J18 Influenza and pneumonia
- J20–J22 Other acute lower respiratory infections
- J30–J39 Other diseases of upper respiratory tract
- J40–J47 Chronic lower respiratory diseases
- J60–J70 Lung diseases due to external agents
- J80–J84 Other respiratory diseases principally affecting the interstitium
- J85–J86 Suppurative and necrotic conditions of lower respiratory tract
- J90–J94 Other diseases of pleura
- J95–J99 Other diseases of the respiratory system
=Symbols
Data sources
Tables in this article use the following notation:
| Value in italics | estimate or provisional data; |
| Value is : | not available.
<context> ContextThere are many factors that can play a role in affecting the health of a person’s respiratory system. Most of these are linked to lifestyle or environmental factors, such as smoking or pollution. Indeed, smoking tobacco is the main cause of lung disease in Europe (note that the data presented in this article do not cover cancer; for further information, see an article on specific cancers), while it is also considered to be a major contributory factor to the incidence of chronic obstructive pulmonary disease (COPD) and the development of asthma in children and adults; furthermore, respiratory diseases also occur among those who are subject to passive smoking. According to the European health interview survey, 19.3 % of people in the EU aged 15 years and over were daily smokers of tobacco products in 2019. Among males, this share was 23.4 % while among females it was 15.5 %. EU Member States have taken various tobacco control measures in the form of legislation, recommendations and information campaigns in an attempt to reduce the number of smokers. From a public health perspective, these measures aim to protect citizens from the hazardous effects of smoking and other forms of tobacco consumption. Air pollution is a major respiratory health issue: activities involving the burning of fossil fuels, such as some industrial activities, power generation, vehicle emissions and household heating/cooking, as well as natural phenomena (such as volcanic eruptions or dust storms) have the potential to cause respiratory diseases. Most sources of outdoor air pollution are beyond the control of individuals and require action by urban, national or international policymakers. Countries that reduce air pollution are likely to benefit from a reduced burden from heart disease, lung cancer, chronic and acute respiratory diseases (including asthma). In urban areas, policies that can potentially alleviate air pollution include support for cleaner transport (including the introduction of low emission zones), energy-efficient housing, or better municipal waste management, while in rural areas air pollution may be alleviated by reducing agricultural waste incineration, forest fires and certain agro-forestry activities. Indoor air pollution is also generated by a variety of sources, including human activity (smoking, fuel used for heating or cooking, the use of cleaning materials), pets, plants, dust or damp, and may be exacerbated by poor ventilation. Influenza is an annual, seasonal infectious disease caused by the influenza virus; it affects Europe in the winter. The majority of people who die from influenza are aged 65 years and over and face complications based on chronic diseases such as cardiovascular diseases or chronic lung diseases. During an influenza epidemic, there may be significant costs for health services (associated with caring for those who fall sick) and for businesses in general (lost production because of time taken off work). The category of chronic respiratory diseases is one of the five main strands covered by the European Commission’s Healthier together – EU non-communicable diseases (NCD) initiative. The initiative was launched in December 2021 and aims to support EU Member States in identifying and implementing effective policies and actions to reduce the burden of major non-communicable diseases and improve citizens’ health and well-being. </context> Explore further
|
link





