Real-world burden of primary hyperoxaluria with chronic kidney disease in the United States: a retrospective administrative claims analysis | BMC Nephrology

Disease epidemiology and characterization of PH
Based on claims with a PH diagnosis in the CMS Medicare FFS LDS and MarketScan CCAE datasets between January 1, 2020 and December 31, 2021, the study sample included 326 patients who had PH (Fig. S1). Applying the projection factors to the US population, an estimated 4500 patients (95% CI 3400–5600) had a diagnosis of PH in 2021. Among these patients, 37% were estimated to have PH with CKD, leading to a projected population of approximately 1600 patients (95% CI 1400–1900). The estimated distribution of CKD by stage indicated that 65% of patients had early stage CKD (stages 1–3) and 33% had advanced stage CKD (stages 4–5), with the CKD stage reported as unknown in 2% of patients.
Median (Q1 – Q3) age was 57 years (42–85) and 63 years (54–71) in all patients who had PH and in those with PH with CKD, respectively, and the projected age distribution showed that patients who had PH with CKD tended to be older than those with PH alone (Fig. 1). The projected gender distribution suggested a slightly higher proportion of male patients, regardless of comorbid CKD stage, although a larger proportion of females than males had PH with advanced CKD.
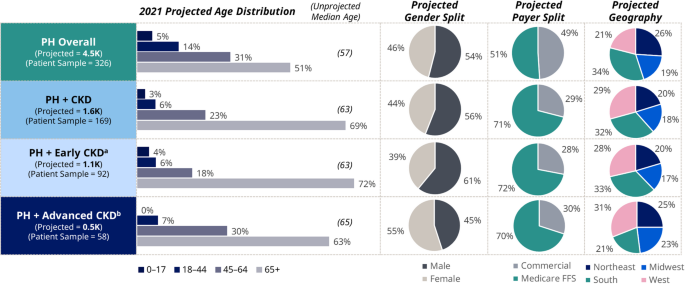
Projected demographics of patients who had PH and PH with CKD. aEarly CKD includes patients who had CKD stages 1–3. bAdvanced CKD includes patients who had CKD stages 4–5 or end stage kidney disease. CKD = chronic kidney disease; FFS = fee for service; PH = primary hyperoxaluria
Unmatched burden of illness analysis
Patients who had PH with CKD showed higher rates of comorbidities and higher rates of treatment than patients who had PH alone. Median CCI scores (Q1 – Q3) were 3.0 (2–4) and 4.0 (2–5) in patients who had PH with early or advanced CKD, respectively, compared with 0.0 (0–1) in patients who had PH alone.
Patients who had PH with early CKD had the highest rates of kidney stone events; within the 6-month period, a higher proportion of patients who had PH with early CKD reported at least one kidney stone event, and among those with kidney stones, a higher proportion had three or more events than patients who had PH alone or PH with advanced CKD (Fig. S2). Analysis of claims for treatments showed that patients who had PH with early CKD had higher pharmacotherapy treatment rates than patients who had PH with advanced CKD, particularly with potassium citrate. Conversely, patients who had PH with advanced CKD were more likely to undergo procedural interventions, including dialysis and kidney transplant (Fig. S3).
No patient claims reported treatment with pyridoxine (vitamin B6; although over-the-counter B6 use was not captured in the dataset), peritoneal dialysis, or liver transplant. No records showed claims for lumasiran treatment, which may be related to the timing of FDA approval of lumasiran (November 2020) and the study period (January 1, 2020 and December 31, 2021).
Patients who had PH with CKD, regardless of stage, had a higher frequency of visits in the outpatient and inpatient hospital setting and similar rates of ER visits when compared with those who had PH alone (Fig. S4). Compared with the other cohorts, the percentage of patients who had PH with advanced CKD reporting at least one visit was higher for specialist visits in the outpatient and inpatient settings and non-specialists in the inpatient setting. Additionally, patients who had PH with advanced CKD had higher mean numbers of specialist and non-specialist visits in the outpatient and inpatient settings than those in the other cohorts.
Patients who had PH with advanced CKD had a greater healthcare cost burden, which was proportional to the higher frequency of outpatient and inpatient hospital visits (Table 1). The mean total healthcare costs in patients who had PH with advanced CKD (mean [SD]: $77,371 [$100,082]) were 10-fold higher than in patients who had PH alone (mean [SD]: $8,080 [$13,620]), and 2.8-fold higher than in patients who had PH with early CKD (mean [SD]: $27,260 [$49,848]); median (range) costs demonstrate the variability of costs in the population. Costs of outpatient/physician office visits were particularly high for patients who had PH with advanced CKD (mean [SD]: $50,761 [$65,390]) compared with outpatient/physician office costs in those who had PH with early CKD (mean [SD]: $11,171 [$19,154]) and patients who had PH alone (mean [SD]: $3,894 [$6,389]). Hemodialysis resulted in a mean (SD) cost of $48,970 ($72,600) in patients who had PH with advanced CKD, $0 in patients who had PH and early CKD (no patients on hemodialysis), and $135 (N/A; median: $135; one patient on hemodialysis) in patients who had PH alone. Patients who had PH with advanced CKD had a median (Q1 – Q3) of 124 (80–179) hemodialysis procedures across the 6-month observation period (equivalent to approximately 5 times per week; data not shown). A total of 14 patients underwent kidney transplant, most of whom were in the PH with advanced CKD cohort (n = 9; n = 4 in the PH with early CKD cohort; n = 1 in the PH alone cohort). The cost of kidney transplant were higher in the PH with advanced CKD cohort (mean [SD]: $80,506 [$93,018]), compared with the PH with early CKD (mean [SD]: $64 [$34]) and PH alone (mean [SD]: $166 [N/A]) cohorts; however, the data should be interpreted with caution because of the low numbers of kidney transplants in each group.
Matched analysis of burden of illness
Patients who had CKD alone (n = 845) were matched with patients who had PH with CKD (n = 169) by age group, gender, CKD stage, and year-month of CKD diagnosis of data assessment (Fig. S5). The largest proportion of patients was in the 45–64 years age group (60%). The majority (66–67%) of patients were female, and most patients had a diagnosis of CKD stage 3 (34–37%) or CKD stage 5/ESKD (29%). Stage was unspecified in 10% and 11% of patients, respectively.
The matched analysis of PH comorbidities showed that patients who had PH with CKD were significantly more burdened with kidney stones (p < 0.01) than patients who had CKD alone, regardless of CKD stage (Fig. 2). In addition, patients who had PH with early CKD were more likely to experience UTIs (p < 0.01) than those with early CKD alone. CCI scores were comparable across the early and advanced CKD cohorts, with median values of 3.0 (Q1–Q3: 1.0–4.0) in patients who had early CKD with or without PH and 4.0 (Q1–Q3: 2.0–6.0) in patients who had advanced CKD with or without PH.
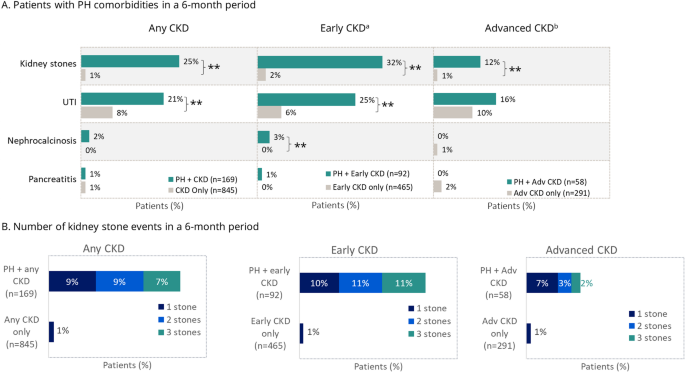
Matched analysis of PH comorbidities in patients who had PH with CKD and CKD alone. **p < 0.01; *p < 0.05. aEarly CKD includes patients who had CKD stages 1–3. bAdvanced CKD includes patients who had CKD stages 4–5 or end stage kidney disease. Adv = advanced; CKD = chronic kidney disease; PH = primary hyperoxaluria; UTI = urinary tract infection
In general, higher rates of pharmacotherapy and medical treatments were observed in patients who had PH with CKD versus matched control cohorts (Fig. 3). Patients who had PH with CKD had higher use of pharmacotherapy than their matched control cohorts; the difference was significant for potassium citrate use, regardless of CKD stage (p < 0.01). With the exception of 4 patients who had PH and early CKD who underwent kidney transplant, dialysis and kidney transplant were generally only used in patients who had advanced CKD. Dialysis was observed in a significantly higher proportion of patients who had PH with advanced CKD compared with those who had advanced CKD alone.

Matched analysis of treatment in patients who had PH with CKD and CKD alone. **p < 0.01; *p < 0.05. aEarly CKD includes patients who had CKD stages 1–3. bAdvanced CKD includes patients who had CKD stages 4–5 or end stage kidney disease. Adv = advanced; CKD = chronic kidney disease; PH = primary hyperoxaluria
Patients who had PH with CKD tended to show higher HCRU than patients who had CKD alone (Fig. 4). The proportions of patients who had healthcare visits for any reason were generally similar between cohorts. Although a larger proportion of patients who had PH with CKD had inpatient hospital stays than those with CKD alone, the mean length of stay tended to be longer for patients who had CKD alone, regardless of CKD stage. Patients who had PH with early CKD had higher rates of specialty visits than the matched patients who had early CKD alone, with significant differences in the mean proportion of patients who had outpatient/physician office visits (p < 0.01) and other specialty care (p = 0.01). Patients who had PH with early CKD were also more likely to visit the ER than patients who had early CKD alone, although this difference was not statistically significant. The mean frequency of outpatient/physician office visits was significantly higher for patients who had PH with early CKD than for patients who had early CKD alone (p < 0.01); this pattern applied to both outpatient/physician office visits and other visits.

Matched analysis of resource utilization in patients who had PH with CKD and CKD alone. (A) Proportions of patients who had at least one healthcare visit for any cause within the 6-month observation window (all-cause healthcare visits). (B) Proportions of patients who had at least one specialty visit for any cause within the 6-month observation window (all-cause specialty visit). (C) Mean number of all-cause healthcare visits within the 6-month observation window. **p < 0.01; *p < 0.05. aEarly CKD includes patients who had CKD stages 1–3. bAdvanced CKD includes patients who had CKD stages 4–5 or end stage renal disease. cOther includes home health, independent labs, and skilled nursing facilities. Adv = advanced; CKD = chronic kidney disease; PH = primary hyperoxaluria
Mean all-cause healthcare costs per six-month period, per patient, in the outpatient/physician office setting were significantly higher for patients who had PH with early CKD versus early CKD alone (p < 0.05) (Fig. 5). Median costs followed the same pattern but demonstrated large ranges in costs, although they were not evaluated statistically. All-cause healthcare costs tended to be similar between patients who had PH with advanced CKD and those who had advanced CKD only. Overall, total median healthcare costs were approximately 1.5-times greater for patients who had PH with CKD than for patients who had CKD alone, regardless of CKD stage (1.8-times greater for PH with early CKD; 1.5-times greater for PH with advanced CKD).

Median total all-cause costs and costs associated with specific visits for six-month period, per patient, in patients who had PH with CKD and matched cohort of patients who had CKD alone. Bar graph represents the median (Q1, Q3) costs, with mean costs in italics. *p < 0.05 for mean values. aEarly CKD includes patients who had CKD stages 1–3. bAdvanced CKD includes patients who had CKD stages 4–5 or end stage kidney disease. cOther includes home health, independent labs, and skilled nursing facilities. CKD = chronic kidney disease; PH = primary hyperoxaluria
link





